Problem Solved: Goodbye to ED "Code Black"
Sweeping nurse understaffing -- and the harm it causes -- back under the rug.
Last week’s big NZ Health story was that Whangarei hospital's emergency department was closed to taking new patients because it hit “Code Black”.
https://www.nzherald.co.nz/nz/whangarei-hospital-ed-hits-code-black-no-new-patients-accepted/EQ2CXVE2AJGATOU54RM77GMEBE/
“Code Black”, in layman's terms, is a situation where the ED is overloaded and no longer functioning safely. The article stated that the ED was at 150% capacity.
The average person would think these things were really bad.
The average person would be right.
The article said that the emergency department had to stop taking new patients because it was in “Code Black”. Of course this wasn't exactly true because NZ emergency departments can never actually shut down due to over capacity.
The most they can do is request regional hospitals not transfer patients to them, maybe divert ambulances elsewhere if there's another hospital to divert to, or possibly they can shut down elective surgeries so that their wards and ICUs are less full.
But they can't ever really close down. They certainly can't say no to a sick patient who needs help.
The story was later edited with a clarification. The Health Minister and others came out saying, correctly, that the ED was never closed.
https://www.teaonews.co.nz/2024/08/17/we-never-turn-people-away-te-whatu-ora-hits-back-at-false-claims-over-whangarei-hospital-code-black/
Then they went a step too far and said, essentially, that things were not that bad, patients were not at risk, and that code black happened regularly.
And while it's true that EDs hit code black regularly, that's not a good thing. It's a tragedy.
It means that on a regular basis, our EDs are becoming overwhelmed by too many patients coming in (sick enough to require admission) without enough nurses on the wards to take care of them.
Researchers call this ‘bed block’ or ‘access block’, a fancy way of saying that there's not enough nurses employed on the wards.
It means that very sick patients requiring admission end up lying in the ED for 6, 12 or even 24 hours blocking up 10-50% of all ED beds.
When this happens (and indeed it happens regularly) it's like your ED has shrunk by 50%. It means that there's physically no available beds to put the next sick patient into.
And that means sick and sometimes even critically ill patients must stay out in the waiting room, or in a corridor, getting substandard and delayed care, because there's physically not a bed space to move them into in the ED.
The answer is not rocket science: ward nurses must be hired to take care of these sick patients. There is no tricky way around it.
Chronic nurse understaffing is just a nonsense that hurts people. And costs us much more in the long run.
The Code Black discussion this week was an important one because clinicians have increasingly been trying to draw attention to the fact that ED overcrowding harms patients.
Indeed it kills patients.
If you can't get timely treatment for your MI, you will have worse outcomes. We know this is the case for not just heart attacks but also a raft of other serious conditions like sepsis, strokes, and heart failure. Delayed care kills people.
The medical literature suggests that for every 82 people whose admission is delayed by 6 to 8 hours, one will die.
https://emj.bmj.com/content/39/3/168
Could someone go through and add up the number of patients who have suffered 8 hour, 12 hour, or 24 hour ED delays, and calculate an “ED delay death rate”? Absolutely, one could do this.
But no one does.
Leaders would argue that an ‘association’ between an excess death and a prolonged ED delay does not prove ‘causation’. It doesn't prove that A causes B.
Yet, the clinicians know that their M&M meetings regularly discuss cases where preventable harm has occurred.
We understand that bed block (which in most cases is just another word for ‘Nurse Understaffing’) kills patients.
And so it was good that attention was drawn to issues of understaffing bed block and code black.
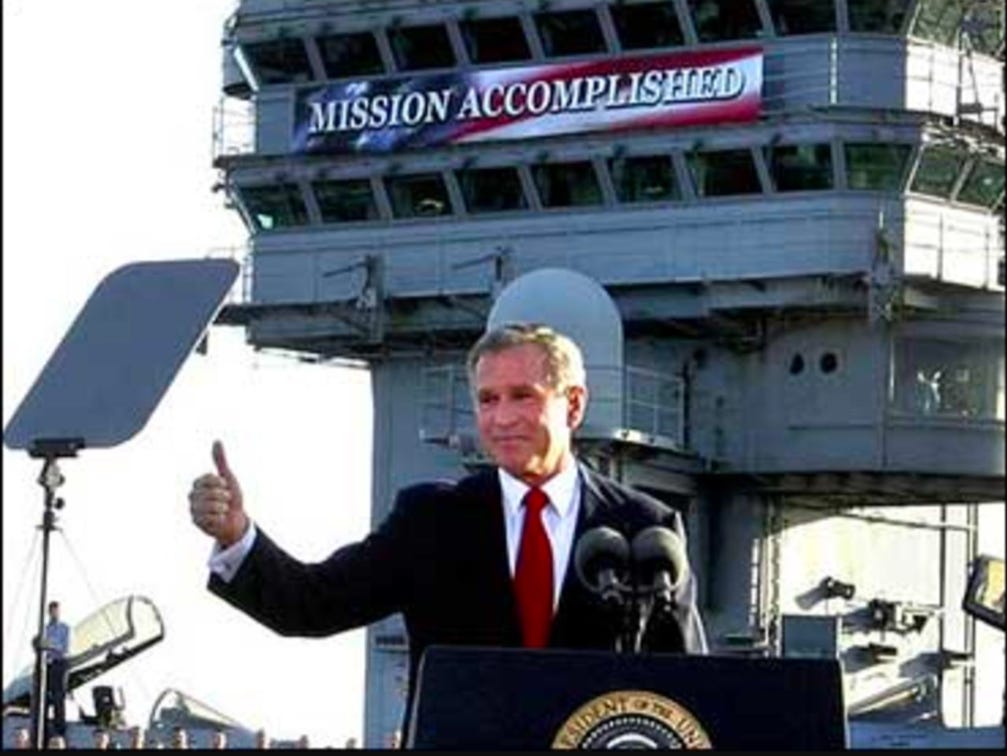
My facetious reply last week was that there's an easy solution to code blacks now that leaders are being made to feel pressure: simply get rid of ‘code blacks’.
I learnt yesterday that this is exactly what's happening.
Nationally ‘code blacks’ are being redefined as firearms incidents. And places that used code black to mean the ‘ED is stuffed’ will have to stop using that term.
The leaders would argue that standardisation of the code colours is a good thing. And it is. But it's also a convenient thing, especially if the new code colours don't address hospital nurse understaffing.
We have to have a robust means of tracking which EDs are collapsing. ‘Code Black’ data was exactly that despite criticisms to the contrary.
If you read that an emergency department was going into code black four or five times a week, it meant something.
It was more than just an “association” between ED overload and “bad outcomes”.
And at the end of the day, the whole reason we're in this job is to prevent “bad outcomes”.
Because a “bad outcome” means some child waiting 6 hours in the waiting room with undiagnosed meningitis will die unnecessarily.
And it means someone's grandfather will die unnecessarily after spending 12 hours in an ED cubicle (with four or six patients to one nurse) rather than an intensive care unit (with one-to-one nursing care).
‘Code Black’ meant something.
‘Code Black’ may be gone but the problem isn't.
-Gary Payinda


Having just been for a week in Dunedin’s hospital following major abdominal surgery, I can relate to the nurse shortages. The staff are wonderful, caring people. I have received outstanding dedication from them. But, a crazed government policy is treating them abominably.
Delayed pay rises, withholding holiday back pay which is agreed needs to be paid, pressure to cover for colleagues and a genuine feeling they are being attacked for just being there underlies their dedication.
Quite why it is seen as acceptable to give tax to landlords, stop building new houses to keep houses expensive, pay tax payers money to corporates and ignore the increasing cost of living whilst underfunding our health service makes me so mad!
On another note, looking at my fellow inmates, I am appalled at the lack of care some people have for themselves. Lack of exercise, poor food habits, obesity etc is, I am sure a major increasing problem for the health service.
I have paid particular attention to walking regularly for the last 20 or so years and the benefit for me is that although having some months of problems, I am now getting mobile after a major surgery relatively quickly.
So, a plea to you all, do please take care of yourself and enjoy life as we are only here once!
Many thanks to the doctors and nurses working hard to treat as many as possible in a difficult situation
Thank you 🙏